The rationale behind my different approach to thyroid management
By Fred Hui, M.D.
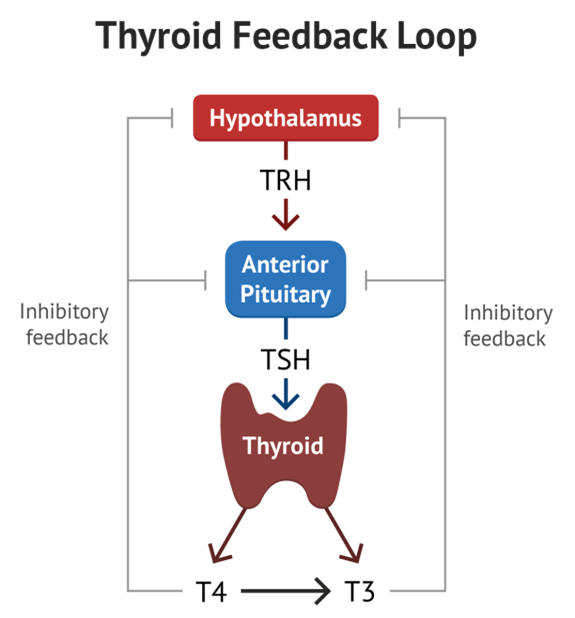
Traditional teaching in medical school is to use Thyroid Stimulating Hormone (TSH) as a marker for whether the thyroid is functioning well. TSH is made by the pituitary glands, which act as sensors for circulating thyroid hormone. If the thyroid is underactive, the pituitary makes MORE TSH, thus providing a clue that the thyroid is underactive. If the thyroid is overactive, the pituitary makes LESS TSH. But that is assuming the pituitary is functioning properly. That is an acceptable assumption in young and healthy patients.
From: “Thyroid Physiology”.MedSchool. https://medschool.co/tests/tft/thyroid-physiology (2020)
Unfortunately, this assumption breaks down in many patients. As an analogy, if you have a supervisor (pituitary) and an employee (thyroid), the supervisor will yell at the employee if they are underperforming. However, if the supervisor themselves are also lazy, the supervisor will not sound the alarm bells when the employee is slow. Thus, everything looks “OK”, when it is in fact not. Similarly, by just looking at TSH from the pituitary (the “supervisor’s” message”), you can understand how it is not a foolproof way for estimating thyroid function.
Therefore, when patients feel symptoms of low thyroid such as tiredness, weight gain and cold intolerance, it is not good enough to just look at TSH. Even when a patient is on replacement of thyroid (such as synthroid or L-thyroxine), it is not enough to just look at TSH.
To go one step further, I like to evaluate both T3 and T4. T3 is the active form of thyroid hormone, whereas T4 is the form it is stored in and is not active. T4 is converted to T3 in the peripheral tissues. The problem is that many conditions can decrease your body’s ability to convert T4 to T3, such as certain mineral deficiencies, abnormal cortisol levels, and abnormal sex hormone levels.
For patients who are feeling well on their existing T4 replacement, I leave them alone. But certain patients, especially those who have been on thyroid supplementation for years, do not feel well on their thyroid supplementation and still feel symptoms of low thyroid despite their TSH and their T4 looking normal. Their MD tells them that their thyroid bloodwork is normal, yet they feel far from it.
From my perspective, these patients are not converting their T4 to T3 and thus do not have enough active thyroid hormone. I treasure looking at the free T3 lab value, I find that it correlates extremely well with the patients’ symptoms. Most physicians do not measure T3.
Ideally, I aim to use natural dessicated thyroid (a combination of T4 and T3), and aim for the upper quarter of the range of normal. It is like tuning up a car, I want my patients to be high functioning. I monitor closely for symptoms of excess replacement.
Sometimes, replacing T3 can lead to a low TSH. Some doctors might panic and think that we are over replacing. The problem is, the brain’s T3 receptors seem to be quite responsive to external T3 containing products and as soon as replacement comes in, they often say that “we are happy and full already”. They stop shouting towards the thyroid gland and send out low TSH. But the peripheral tissue receptors are less sensitive and may not have enough. As long as T4 and T3 are not elevated and there are no clinical symptoms or signs of over replacement, I continue to monitor very carefully.
In my experience, paying attention to T3 and replacing with a combination of T3/T4 makes a significant difference in the lives of patients.
Below are some articles in line with my approach:
How Accurate is TSH Testing? – National Academy of Hypothyroidism
Why dessicated thyroid is better than synthetic thyroid